Causal Agent:
Toxoplasma gondii is a
protozoan parasite that infects most species of warm blooded animals, including humans,
and can cause the disease toxoplasmosis.
Life Cycle:

The only known definitive hosts for Toxoplasma gondii
are members of family Felidae (domestic cats and their relatives).
Unsporulated oocysts are shed in the cat’s feces
 .
Although oocysts are usually only shed for 1-2 weeks, large numbers may be
shed. Oocysts take 1-5 days to sporulate in the environment and become
infective. Intermediate hosts in nature (including birds and rodents)
become infected after ingesting soil, water or plant material contaminated
with oocysts .
Although oocysts are usually only shed for 1-2 weeks, large numbers may be
shed. Oocysts take 1-5 days to sporulate in the environment and become
infective. Intermediate hosts in nature (including birds and rodents)
become infected after ingesting soil, water or plant material contaminated
with oocysts
 .
Oocysts transform into tachyzoites shortly after ingestion. These
tachyzoites localize in neural and muscle tissue and develop into tissue
cyst bradyzoites .
Oocysts transform into tachyzoites shortly after ingestion. These
tachyzoites localize in neural and muscle tissue and develop into tissue
cyst bradyzoites
 .
Cats become infected after consuming intermediate hosts harboring tissue
cysts .
Cats become infected after consuming intermediate hosts harboring tissue
cysts
 .
Cats may also become infected directly by ingestion of sporulated oocysts.
Animals bred for human consumption and wild game may also become infected
with tissue cysts after ingestion of sporulated oocysts in the environment .
Cats may also become infected directly by ingestion of sporulated oocysts.
Animals bred for human consumption and wild game may also become infected
with tissue cysts after ingestion of sporulated oocysts in the environment
 .
Humans can become infected by any of several routes: .
Humans can become infected by any of several routes:
- eating undercooked meat of animals harboring tissue
cysts
 . .
- consuming food or water contaminated with cat feces
or by contaminated environmental samples (such as
fecal-contaminated soil or changing the litter box of a pet cat)
 . .
- blood transfusion or organ transplantation
 . .
- transplacentally from mother to fetus
 . .
In the human host, the parasites form tissue cysts, most
commonly in skeletal muscle, myocardium, brain, and eyes; these cysts may
remain throughout the life of the host. Diagnosis is usually achieved
by serology, although tissue cysts may be observed in stained biopsy
specimens
 .
Diagnosis of congenital infections can be achieved by detecting T. gondii
DNA in amniotic fluid using molecular methods such as PCR .
Diagnosis of congenital infections can be achieved by detecting T. gondii
DNA in amniotic fluid using molecular methods such as PCR
 . .
Geographic
Distribution:
Serologic prevalence
data indicate that toxoplasmosis is one of the most common of humans infections throughout
the world. A high prevalence of infection in France
has been related to a preference for eating raw or undercooked meat, while a high prevalence
in Central America has been related to the frequency of stray cats in a climate favoring
survival of oocysts and soil exposure. The overall seroprevalence in
the United States among adolescents and adults, as determined with specimens
collected by the third National Health and Nutrition Examination Survey
(NHANES III) between 1988 and 1994, was found to be 22.5%, with a seroprevalence among women of
childbearing age (15 to 44 years) of 15%.
Diagnosis

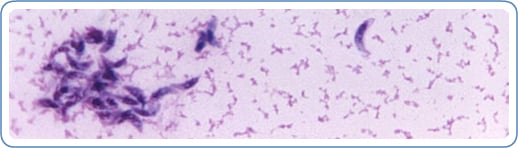
A Toxoplasma-positive reaction, stained by immunofluroescence (IFA). (CDC Photo)
The diagnosis of toxoplasmosis is typically made by serologic
testing. A test that measures immunoglobulin G (IgG) is used to
determine if a person has been infected. If it is necessary to try to
estimate the time of infection, which is of particular importance for
pregnant women, a test which measures immunoglobulin M (IgM) is also
used along with other tests such as an avidity test.
Diagnosis can be made by direct observation of the parasite in
stained tissue sections, cerebrospinal fluid (CSF), or other biopsy
material. These techniques are used less frequently because of the
difficulty of obtaining these specimens.
Parasites can also be isolated from blood or other body fluids (for
example, CSF) but this process can be difficult and requires
considerable time.
Molecular techniques that can detect the parasite's DNA in the
amniotic fluid can be useful in cases of possible mother-to-child
(congenital) transmission.
Ocular disease is diagnosed based on the appearance of the lesions in
the eye, symptoms, course of disease, and often serologic testing.
rest
Prevention & Control
People who are healthy should follow the
guidelines below to reduce risk of toxoplasmosis. If you have a weakened
immune system, please see guidelines for Immunocompromised Persons.
Reduce Risk from Food
To prevent risk of toxoplasmosis and other infections from food:
- Cook food to safe temperatures. A food thermometer should be used
to measure the internal temperature of cooked meat. Do not sample meat
until it is cooked. USDA recommends the following for meat preparation.
- For Whole Cuts of Meat (excluding poultry)
- Cook to at least 145° F (63° C) as measured with
a food thermometer placed in the thickest part of the meat, then allow
the meat to rest* for three minutes before carving or consuming.
- For Ground Meat (excluding poultry)
- Cook to at least 160° F (71° C); ground meats do not require a rest* time.
- For All Poultry (whole cuts and ground)
- Cook to at least 165° F (74° C), and for whole poultry allow the meat to rest* for three minutes before carving or consuming.
*According to USDA, "A 'rest time' is the
amount of time the product remains at the final temperature, after it
has been removed from a grill, oven, or other heat source. During the
three minutes after meat is removed from the heat source, its
temperature remains constant or continues to rise, which destroys
pathogens."
- Freeze meat for several days at sub-zero (0° F) temperatures before cooking to greatly reduce chance of infection.
- Peel or wash fruits and vegetables thoroughly before eating.

Wash counter tops carefully. Photo courtesy of USDA.
- Wash cutting boards, dishes, counters, utensils, and hands with hot
soapy water after contact with raw meat, poultry, seafood, or
unwashed fruits or vegetables.
The U.S. Government and the meat industry continue their efforts to reduce T. gondii in meat.
Reduce Risk from the Environment
To prevent risk of toxoplasmosis from the environment:
- Avoid drinking untreated drinking water.
- Wear gloves when gardening and during any contact with soil or
sand because it might be contaminated with cat feces that contain Toxoplasma. Wash hands with soap and warm water after gardening or contact with soil or sand.
- Teach children the importance of washing hands to prevent infection.
- Keep outdoor sandboxes covered.

Have someone else clean the litter box. (CDC Photo)
- Feed cats only canned or dried commercial food or well-cooked table food, not raw or undercooked meats.
- Change the litter box daily if you own a cat. The Toxoplasma parasite
does not become infectious until 1 to 5 days after it is shed in a
cat's feces. If you are pregnant or immunocompromised:
- Avoid changing cat litter if possible. If no one else
can perform the task, wear disposable gloves and wash your hands with
soap and warm water afterwards.
- Keep cats indoors.
- Do not adopt or handle stray cats, especially kittens. Do not get a new cat while you are pregnant
by :hayu
|
|








0 komentar:
Posting Komentar